|
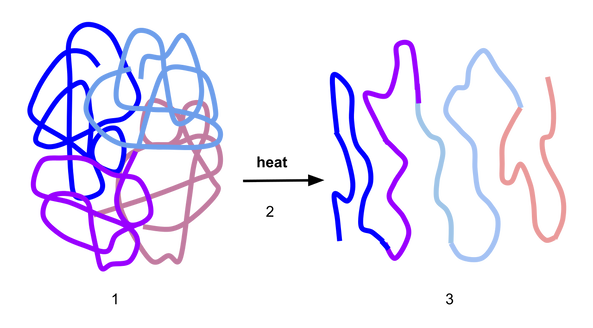
Children are still enjoying the summer holidays, but the schools are due to re-open their doors in September and I’m very conscious that I will soon be inundated with calls from concerned parents and letters from GPs or practice nurses with the same old question I get every year. “My child has an allergy to egg; can they have the flu vaccine?” and “this child needs a flu vaccine to be administered in a hospital due to having an egg allergy.” The fact is that there are very few individuals who cannot receive any influenza vaccine. The Department of Health guidelines state that none of the influenza vaccines should be given to those who have had: either a confirmed anaphylactic reaction to a previous dose of the vaccine, difficult to manage asthma, or a confirmed anaphylactic reaction to any component of the vaccine. So, if your child has none of these, then they can have their annual flu vaccine. If you are still concerned, talk to your GP. If an egg-free vaccine is not available, they should be able to advise you about a suitable vaccine with very low egg content. Sometimes, based on a child’s previous medical history, your GP may refer your child to the hospital to have a flu vaccine. This requires prior consultation with an allergy consultant and when appropriate, booking a day in the hospital where the child will be given a skin prick test. If the test is negative, part of the vaccine is given first and after a period of observation, the rest of the vaccine is administered. A little science: With egg allergy (as with all food allergies), we are concerned about the body’s mistaken immune response to the proteins in the egg which are: ovalbumin, ovotransferrin, ovomucoid, ovomucin and lysozyme. Ovalbumin is the major protein in egg white and it’s heat resistant - meaning that even when processed - sometimes egg still cannot be tolerated by individuals with egg allergy. Other egg proteins such as ovomucoid can be denatured by the heat. As a result, the shape of the protein changes (see the figure below) and increases the likelihood of tolerance. Inactivated influenza vaccines are egg-free or have extremely low ovalbumin content. For example, the Quadrivalent Influenza Vaccine (split virion, inactivated) manufactured by Sanofi Pasteur®, contains 0.12 micrograms/ml which is equivalent of a 0.05 microgram in 0.5 ml dose. Evidence shows that even LAIV manufactured by Fluenz Tetra® which previously had a higher content of ovalbumin of 1.2 micrograms/ml was also safe when given to children with egg allergy. LAIV now contains a significantly reduced ovalbumin content of a £ 0.024 microgram in a 0.2 ml dose. The Green Book is a document issued by the Department of Health about vaccines and every year, an update is issued about available vaccines and all relevant guidelines applicable to those vaccines. Your GP should have received their copy and will able to offer the best vaccine for your child. References:
1. Does food allergy cause eczema?
Eczema and allergy are two separate diseases. Eczema is a primary disease and food allergy does not cause eczema. Eczema usually presents itself in the first few months of life. Nevertheless, infants, toddlers and children with eczema can develop a food allergy too. As a result, if they consume the food they are allergic to, they will have a flare-up of their eczema. If you have concerns that some foods may cause a repeated flare of your child’s eczema (every time the child consumes the same food), then you may consider asking your GP to refer to an allergy specialist. 2. Can you test for everything so I can find what my child is allergic to? There is no global test for allergy that would tell us that. An allergy is a reproductive reaction to a specific protein in each type of food or environmental allergens. There are so many types of foods and aeroallergens which means it’s impossible to test them all. Instead, we take a detailed history to determine which tests to request. Therefore, your GP will ask you to keep an allergy symptom diary. An allergy diary is helpful to identify the trigger for your child’s reactions and establish an initial diagnosis. It is also useful background information for an allergy specialist. 3. Will my child grow out of their allergy? This depends on the age of the child when we identify the allergy and the type of allergen. When allergy is managed from infancy, some children will likely grow out of it. However, the type of food allergen is a key factor because the reaction is to a specific protein in the food and each food contains a different type of protein. Often, the proteins can be broken down by cooking or processing so the body can slowly accept it. This is often the case for milk and egg. When a small amount of milk is added to food e.g. a baked biscuit, some of the milk proteins are broken down by the heat. There is also a role which the other ingredients play - such as wheat - that also help the process. Introducing gradually small amounts of baked milk tends to be well accepted. The same principle is applied to egg, e.g. one egg added to a recipe for 12 mini muffins. The denatured egg proteins can be well accepted and define the beginning of a better tolerance to egg. However, with an allergy to fish and nuts, for example, heating or processing does not work and instead does exactly the opposite. Roasting nuts, even when mixed in food such as in pastries can make their protein stronger. Therefore, having a close working relationship with an allergy specialist and dietitian is important to ensure a safe and successful outcome. 4. My child has an allergy to egg. Can they have a flu vaccine? Children with an egg allergy may be at risk of an allergic reaction to the flu vaccine because most flu vaccines can contain part of egg protein (ovalbumin). This largely depends on the severity of your child’s allergy to egg and their history of an allergic reaction to other vaccines that may have a similar content (this can be established by your GP). In recent years, egg-free flu vaccines have become available and your GP can find the best option for your child. Sometimes, based on the previous history, your GP may refer your child to the hospital to have their vaccine. This, however, is not just a matter of coming and have the vaccine done. It requires consultation with an allergy consultant and when appropriate, booking a day admission on the ward where the child will have a skin prick test first. If the test is negative, then part of the vaccine is given first followed by the rest. With the fast-approaching new school year and autumn/winter seasons, I have written a more detailed blog post on the flu vaccine and egg allergy which you can read here. 5. My child has an allergy to egg; can they have an MMR vaccine? In 2009, the World Allergy Organisation issued the first memo to all clinicians, reminding them that measles and mumps vaccines are safe to be given to children with egg allergy without any special precautions. The vaccines are grown in chick embryo fibroblast and contain negligible or no egg protein. As with all vaccines, it should not be given to children who have had an allergic reaction to a previous MMR or suffered from anaphylaxis after a negligible amount of egg (e.g. a regular size cake containing one egg). We should remember that the risk of death from Measles is significant and therefore, your child having their MMR vaccine is important. If you have any concerns, seek advice from your GP who can refer you to an allergy specialist. |
AuthorAneta Ivanova Archives
March 2023
Categories |
The Consulting Rooms, 38 Harborne Road, Birmingham, B15 3EB
[email protected]
Website design & content by LIT Communication: www.litcommunication.com
[email protected]
Website design & content by LIT Communication: www.litcommunication.com


 RSS Feed
RSS Feed