|
While food allergies and intolerances can cause some of the same symptoms, there are some key differences between the two. These should help you differentiate between whether your child is suffering from a food allergy or an intolerance, but it’s always best to seek proper testing from a specialist for food allergies from if you suspect that might be the cause.
Digestive system vs. immune system response A food allergy is a negative immune system response to a food protein that triggers an allergic reaction. When an allergy occurs, your immune system overreacts, producing Immunoglobulin E (IgE) antibodies which travel to cells and release chemicals that cause an allergic reaction. 90% of all food allergies are caused by the top-eight food allergens, which includes wheat, soy, shellfish, fish, milk, eggs, soy, peanuts and tree nuts. The other 10% of food allergies can come from any food, with some children allergic to products such as red meat, citrus and celery (for example). Food intolerance, on the other hand, is a negative reaction to a food that doesn’t involve the immune system and instead takes place in the digestive system. Food intolerances are not normally life-threatening. Intolerance reactions normally take much longer to develop (up to 20 hours after consuming food) and occur when your body is unable to digest a certain food properly. Food allergy symptoms vs. food intolerance symptoms A food allergy can cause a potentially life-threatening reaction when the food is touched, eaten or even inhaled. This is referred to as anaphylaxis which normally occurs within seconds or minutes of eating food and symptoms include difficulty breathing, dizziness or losing consciousness. Anaphylaxis requires immediate treatment with an adrenaline shot to prevent fatal consequences, and the symptoms include suddenly feeling weak due to a drop in blood pressure and breathing problems as the throat begins to swell up. Other, nonlife-threatening symptoms of food allergy are either shown on the skin, respiratory or gastrointestinal. The most common symptoms of food allergy include itching, developing a rash or hives. Gastrointestinal symptoms are identified by vomiting or diarrhoea and respiratory symptoms can include shallow breathing, wheezing, chest congestion, coughing, a runny or blocked nose and itchy/watery eyes. In contrast to food allergies, food intolerance symptoms are focused on the digestive system and common symptoms include diarrhoea, bloating and an upset stomach. Less common food intolerance symptoms include weight loss, lack of energy, headaches and anaemia. These symptoms are often linked to other digestive disorders such as Irritable Bowel Syndrome (IBS and Chron’s Disease). Food allergy testing vs. food intolerance testing Food allergy testing can be carried out by an allergy specialist and there are two different ways to test for an allergy. For symptoms that develop quickly (an IgE-mediated food allergy) – a skin prick test or a blood test is the recommended tool for diagnosis. For symptoms that are slowed to develop (a none IgE-mediated food allergy) – a food elimination diet is the best way to diagnose. There are no food intolerance tests that are currently recommended by the British Dietetic Association, so the best way to identify an intolerance is to keep a food diary and monitor your symptoms. If you suspect a certain food is a cause, cut this out of your diet and see whether your symptoms disappear. You can then slowly reintroduce it to see if this causes your symptoms to flare up again. For advice relating to food allergies or intolerances, email me at [email protected] with any questions and I’ll be happy to help. The difference between allergy symptoms and covid-19 symptoms
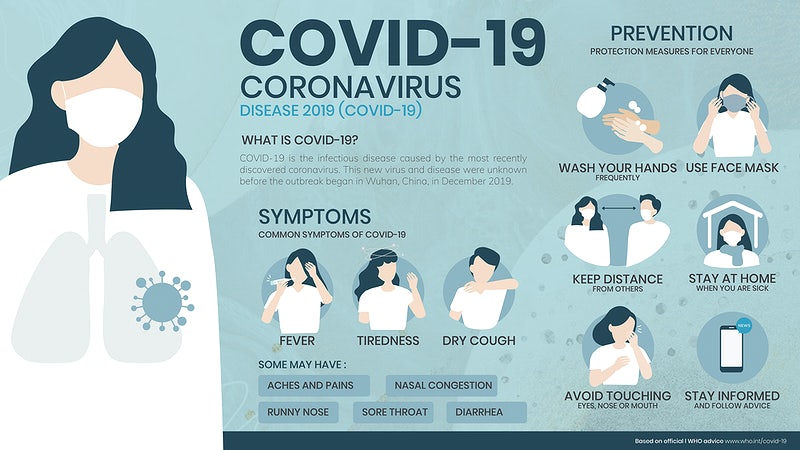
The coronavirus has heighted everyone’s fears when it comes to identifying symptoms – even if these are symptoms that have been experienced previously. The timing of the global covid-19 pandemic has also coincided with the onset of spring which is when many seasonal allergies begin to flare. To help put your mind at ease, we want to help highlight the differences between covid-19 symptoms and the symptoms associated with seasonal or year-round allergies. Covid-19 symptoms Covid-19 symptoms can appear up to two weeks after exposure, and the official symptoms include having a new, continuous cough, presenting a high temperature, physical fatigue and a loss or change to your sense of taste or smell. Although these are the main symptoms, other, less common symptoms have also been reported by coronavirus patients. These lesser-known symptoms include having a fever, sore throat or achiness. Some people have also reported sneezing, digestive issues/discomfort, mental fatigue, chills, nausea and diarrhoea. Seasonal allergy symptoms The key difference between Covid-19 symptoms and the symptoms of seasonal allergies are that you don’t normally get a fever and high temperature if you’re affected by an allergy. The symptoms of seasonal allergy are much more likely to include postnasal drainage, ear congestion, a runny nose and itchiness in various places - such as the eyes, ears, nose and throat. These symptoms are not known to be associated or reported as a symptom of coronavirus. Sneezing is another symptom that sets coronavirus and seasonal allergies apart. If you are just sneezing and do not have a fever or any achiness in the body – it’s most likely to be hayfever that you’re suffering from. Seasonal allergies also cause a non-stop sneeze and irritation, rather than infrequent sneezing which could be a side effect of coronavirus. You will likely see an improvement in your allergy symptoms after taking an antihistamine, so this will be a good indicator that your seasonal allergy has flared up. It’s important to remember that even though you have seasonal allergies, you could still be at risk of catching coronavirus, so should take all the necessary precautions when you’re out and about. Tips to help minimise the risk of catching coronavirus To help keep both your seasonal allergies and coronavirus at bay, you should continue taking your regular, daily allergy medication consistently. If you need to sneeze in public, you should do this as safely as possible, sneezing into a tissue or the corner of your elbow. Current NHS guidelines (on the day of publishing this article) recommend that you stay at home as much as possible, work at home if you can and keep a 2m distance from people when you’re out. For advice on your seasonal allergy symptoms, please email me at [email protected] |
AuthorAneta Ivanova Archives
March 2023
Categories |
The Consulting Rooms, 38 Harborne Road, Birmingham, B15 3EB
[email protected]
Website design & content by LIT Communication: www.litcommunication.com
[email protected]
Website design & content by LIT Communication: www.litcommunication.com


 RSS Feed
RSS Feed